Don't Stuck in the Waiting Room!
Register Online Before You Arrive.
We have up-to-date schedules, contact information, and allow you to make appointments online.
RETROGRADE INTRARENAL SURGERY
All endoscopic methods were initially used for diagnostic purposes and later transitioned to therapeutic use with technological advancements. Flexible ureteroscopy (f-URS) was first reported in 1964 when the obstruction-causing stone in the ureter was visualized [1]. Today, with f-URS, even small staghorn stones can be fragmented into small, passable particles less than 2 mm in size [1]. With continuous technological advancements, smaller diameter endoscopes with high image quality have been produced, and various energy forms have been developed for use in procedures. Nowadays, f-URS is used not only for diagnostics or stone treatment but also in the monitoring and treatment of upper urinary system tumors and the resection of ureteral strictures [2,3]. Table-1 outlines the main uses of f-URS.
A. Flexible Ureteroscopy Technique and Diagnostic Flexible Ureteroscopy:
In diagnostic ureteroscopy, the practice at our clinic involves examining the distal ureter up to the iliac crossover with a semirigid URS following cystoscopy and the placement of a safety wire in the relevant ureter. Then, the scope is changed to f-URS to examine the proximal ureter and the ureteropelvic junction (UPJ). After entering the pelvicalyceal system, contrast media is delivered through the irrigation channel to perform an ascending pyelography under fluoroscopy to map the locations and numbers of the calyces. Systematic control is then performed, starting from the upper calyx group, followed by the middle and lower calyces (Figure 1). Care should be taken to avoid excessive dilation of the pelvis with the pressurized irrigation fluid or contrast given at this time. This could result in iatrogenic submucosal or calyceal fornix bleeding, leading to misdiagnosis.
The first move in the f-URS technique is to bend the distal 2-3 cm portion of the endoscope in two directions with a thumb motion, achieving a 170/120-degree flexion. In addition to this motion, a secondary flexion can be achieved by bracing the distal 5-10 cm of the f-URS against the upper calyx neck in the renal pelvis to enter the lower calyceal system (Figure 1). In 2/3 of patients, this secondary deflection maneuver is necessary to fully visualize the interior of the lower calyceal system. Even in large series reported by experienced hands, it is reported that the lower calyceal system could not be entered in 6% of patients despite these maneuvers [2]. These are usually systems that are highly dilated or have a calyx neck longer than 3 cm.
In a study of 23 patients examining the role of flexible ureteroscopy in evaluating chronic unilateral hematuria, pathology was identified in 78% of patients [3]. Hemangiomas, papillary tumors, venous leaks, and stones are reported as the main causes. Tawfiek’s study reports tumors in 3 out of 23 patients (13%).
Nakada and colleagues report a 5-year success rate of 82% for endoscopic treatment of lateralized hematuria if a distinct lesion can be identified. However, it is noted that in this study, 100% of patients with diffuse lesions and 66% of patients with no identifiable lesions experienced recurrent bleeding [4]. Another study reports a 93% success rate in the endoscopic treatment of renal hemangiomas ranging from 2-10 mm in diameter [5]. In this study, a 2-3 F ball electrode and a 200-micron Holmium laser probe were used for fulguration of the hemangiomas, 40% of which were multiple.
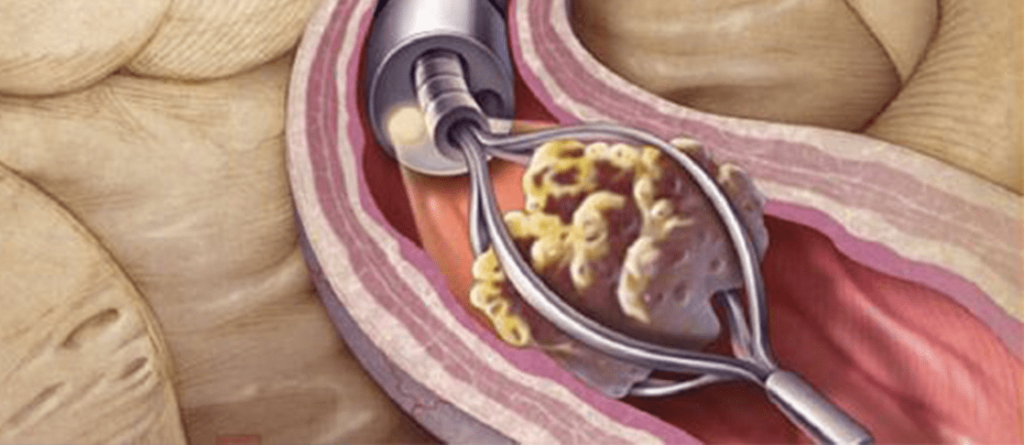
B. Flexible Ureteroscopy in Retrograde Stone Treatment:
In the planning of treatment for upper urinary system stones, the size, location, shape of the stone, and upper urinary system anatomy are important. Currently, for uncomplicated upper urinary system stones smaller than 2 cm with suitable anatomy, ESWL is considered the first-line treatment [6]. These changes have limited the indications for the endoscopic treatment of urinary system stones. However, for large stones that have caused significant obstruction, where fluoroscopic localization is difficult, especially in obese patients, endoscopic methods are the most appropriate treatment [7]. For stones that cannot be fragmented or are very slow to fragment with ESWL, transitioning to endourological treatment will provide minimal morbidity and maximal success rates. Table 2 lists the primary f-URS indications for kidney stones.
One of the most challenging endoscopic procedures is the treatment of lower calyx stones with f-URS. It is quite difficult to focus the end of the endoscope directly on the stone in the lower calyx. Even a 0.2 mm diameter Holmium laser probe can reduce the deflectability of the ureteroscope by 7-16% [8]. When f-URS is angled at 90 degrees or more, advancing any probe through the working channel becomes impossible. Therefore, instead of fragmenting the lower calyx stone in situ, it is easier to reach the stone using primary and secondary deflection maneuvers, grasp the stone with a nitinol basket if it is smaller than 1 cm, and move it to the upper calyx for fragmentation with a Holmium laser. The Duke group reports an 83% success rate for in situ stone fragmentation in the lower calyx and 88% success when stones are moved to the upper calyx for fragmentation [9]. The lower calyx working group reports a 63% stone-free rate for stones smaller than 10 mm and a 23% rate for stones between 10-20 mm with alternative ESWL treatment [10].
The treatment of stones larger than 2 cm and small staghorn stones in the pelvicalyceal system with f-URS has been reported in a series of 48 patients [1]. In this series, the procedure is defined as fragmentation of the stone into small, passable pieces using f-URS and Holmium laser. Complete fragmentation in a single session was achieved in 34/45 (76%) patients, and staged treatment resulted in complete fragmentation in 42/45 (93%) patients. In three patients, standard percutaneous nephrolithotripsy was performed as the stone could not be reached, and the control checks performed at the 6-month follow-up using ultrasound revealed a 24% residual stone (debris?) rate in the lower pole and a 16% rate of new stone formation. The stone-free rate reported in this study is 60%, but no information is provided on the number of f-URS used or any device damage.
The effectiveness of the “access sheath,” which has become popular in recent years, was evaluated in a prospective randomized study, which reported that its use during f-URS reduced operation time and costs, caused minimal morbidity, and recommended its routine use [11]. However, placing a 14 F stent in the ureter to deliver a 7.5 F f-URS to the pelvicalyceal system in each case and the resulting postoperative edema requiring a double-J catheter may be considered a disadvantage. There is literature both supporting and opposing the use of the ‘access sheath.’ In our clinic, the “access sheath” is mostly used in pelvicalyceal system stones if the stone load is high and multiple entries and exits to the ureter are necessary (Figure 2 a and b).
Most of the f-URS used today have a single channel with a diameter of 3.6 F, used for both irrigation and working channels. The inside of this channel is lined with a thin plastic sheath that provides water insulation to the system’s other components. When primary or secondary deflection is performed with f-URS, the round working channel becomes oval. Accessory instruments pushed into the working channel while the device is in flexion, especially the 200-micron Holmium laser probe, perforate the plastic sheath inside the working channel, allowing irrigation and sterilization fluids or gases to leak into the optical system, damaging the device. We believe that half of the f-URS damage in our clinic is caused in this way. Therefore, instead of fragmenting stones, especially lower calyx stones, in situ or transferring them to the upper calyx for fragmentation, our clinic prefers to grasp them with a nitinol basket and pull them into the proximal ureter for fragmentation with a rigid URS [12].
Another working channel damage occurs when f-URS is pushed into the ureter using the ‘monorail’ method. During this time, working wires with stiff proximal ends can damage the channel, so it is appropriate to use hydrophilic wires with soft ends on both sides when performing f-URS.
The instrument used to deliver the desired device to the working area inside the kidney must be thinner than 3 F; ideally 2.5 F. This allows for a space through which irrigation fluid can be delivered for good visualization and minimizes restrictions on the instrument’s flexibility. During this time, using specially designed systems (Pathfinder PlusTM Bulb Irrigator, Utah Medical) to deliver pressurized irrigation fluid can enhance image quality [1]. Especially before long-lasting procedures, it is beneficial to place a 10-12 F Nelaton catheter into the bladder to provide drainage.
In our clinic, we prefer nickel titanium (Nitinol, Zero Tip) baskets with a 12 mm opening and a 2.4 F thick body for stone treatment with f-URS. These baskets minimally restrict f-URS movements, do not cause perforation in the working channel or calyx fornix due to their soft tips, and make it easy to capture and release stones when necessary. Being pre-shaped baskets, even if accidentally cut with a Holmium laser during the procedure, they open like an umbrella, preventing damage to the ureter.
In almost all series in the literature, Holmium laser is used as the energy source for ureterolithotripsy with f-URS. This device, used as a lithotripter since 1995, works on the principle of delivering light energy at a wavelength of 2150 nm to the target area through quartz probes, melting and fragmenting the stone with high heat generated at the probe tip [13]. Coagulation and even perforation in surrounding tissues can occur during Holmium laser lithotripsy [14]. For safety, it is necessary to start the f-URS Holmium laser lithotripsy procedure at low power and gradually increase the energy and frequency based on the stone size and fragmentation status.
Electrohydraulic lithotripsy (EHL) can also be applied using a 1.9 F probe with f-URS. Its disadvantages are the inability to break very hard stones, the risk of tissue damage due to weak energy control, a perforation rate of up to 40%, and the limitation of f-URS movements by the probe in lower calyx stones. Recently, nitinol flexible probes have been produced for pneumatic lithotripters, and some experience with them is documented in publications [15].
When treating proximal ureter stones with rigid or flexible URS, there is a risk of migration. To prevent migration, keep the lithotripter’s firing frequency low, perform the procedure with the patient in the Trendelenburg position to allow the stone to migrate to the upper calyx instead of the lower calyx, and tilt the table to keep the working side uppermost. Additionally, nitinol cone spirals (Stone cone), which open behind the stone to prevent migration, are reported to be effective in preventing migration [16,17]. Due to cost considerations, they are not routinely used in our clinic.
C. Retrograde Treatment of Upper Urinary System Tumors:
Resection or ablation of low-grade, superficial upper urinary system tumors is possible with flexible ureteroscopy. This method may be a suitable treatment option, especially for patients with a solitary kidney, renal failure, or bilateral tumors. Retrograde treatment with f-URS should be considered for treating low-grade, solitary, and less than 15 mm tumors.
Even if indications are limited, approximately 1/3 of patients fail to achieve complete resection of the tumor despite multiple ureteroscopic interventions [18]. No correlation has been reported between tumor location and tumor-free or recurrence rates. Keeley and colleagues report that 36% of tumors larger than 15 mm can be completely resected, while this rate rises to 91% for tumors smaller than 15 mm [19].
The recurrence rate is reported as 37% in the renal pelvis and 43% in the ureter over three years. As in bladder tumors, high-grade tumors have a higher recurrence rate compared to low-grade tumors.
As mentioned in the diagnostic f-URS section, before starting tumor resection, a systematic examination of the collecting system should be completed, and any additional pathology to the existing tumor should be noted. Then, a biopsy should be taken from the tumor for histological examination. For this procedure, Holmium laser, biopsy forceps, or a tripod grasper can be used. In our clinic, 2.4F, 4-wire, sharp-edged Segura basket catheters are preferred due to their ability to take sufficient samples and ease of use. After the biopsy, the tumor base is cauterized, using either a 1.9 F ball electrode or a 200-micron Holmium laser probe. Keeley and his team from Philadelphia report a 97% accuracy in diagnosis of upper urinary system tumors using these techniques [19].
There is still no clear information about using intravesical Mitomycin-C or BCG after ureteroscopic resection in upper urinary system (UUT) tumors. The effect of adjuvant therapy on local recurrence and cancer-specific survival has not been fully proven. However, adjuvant therapy is generally well-tolerated and can be administered by JJ catheter from the bladder through reflux. Another method is administering the drug suprapubically or through a ureteral catheter removed from the urethra. It is reported that this method may have a lower risk of ureteral stricture [20]. There is still no standard regarding drug dosage and administration frequency.
In monitoring patients, flexible cystoscopy every three months and f-URS examination every six months are recommended for the first two years, followed by six-month cystoscopy and annual f-URS [20]. This intensive endoscopy program aims to detect about 40% recurrence early. It is reported that radiological imaging methods fall short during follow-ups and detect recurrences only 25% of the time [21]. The same publication also reports that as long as the tumor’s grade or stage does not increase, it may be possible to treat recurrences with repeated ureteroscopic resection and avoid nephroureterectomy.
One of the primary concerns in the diagnosis and treatment of UUT tumors with f-URS is retrograde pyelolymphatic or pyelovenous migration of tumor cells due to the high-pressure fluid used during the procedure, leading to recurrence and progression. However, the Cleveland group reports that diagnostic URS has no such long-term effect on survival [22]. It is also reported that fluid absorption during f-URS is minimal, and using an access sheath, even with high-pressure irrigation, can keep intrapelvic pressure at 20 cm H2O [23,24].
The standard treatment for upper urinary collecting system tumors is open or laparoscopic nephroureterectomy performed according to oncological principles. As stated at the beginning of this section, it should be remembered that patients suitable for treatment with f-URS are selected patients with superficial, low-grade small tumors who can adhere to close follow-up and mostly require nephron preservation for compelling reasons.
D. Complications and Cost
Indications for retrograde intrarenal surgery have expanded today, and the number of reported cases has increased. The diameter reduction of the main equipment, f-URS, the increase in image quality, the experience in this field, and the use of effective and safe auxiliary instruments such as Holmium laser and nitinol baskets have significantly reduced complication rates in interventions. Blute25 reported a 7.5% rate of major complications such as avulsion, major perforation, stenosis, urinoma, and urosepsis in a series of 346 patients in 1988, but this rate decreased to 0.7% in a series of 1000 patients in 2000 [25,26].
The inability of flexible ureterorenoscopy to become routine in clinical practice in our country is perhaps most importantly due to their fragility and frequent need for repair. It is reported that there is not much difference in durability between models, and major damage occurs in an average of 10 to 15 uses, requiring repair abroad [27]. In our clinic’s first published series, this rate was 2 in 31 uses [12]. Since the average repair cost is between $3,500 and $5,500, using f-URS adds an additional cost of about $300-400 per patient. It is reported that new generation ureteroscopes with a 6.75 tip, 9.0 F body, and secondary deflection capabilities are more durable, offer usage advantages, and do not require repair for up to 35 uses [28,29].
Retrograde intrarenal surgery can be applied effectively and safely in diagnosing and treating upper urinary system pathologies. The fragility of f-URS and the resulting increased cost are the main problems in practice.
DO YOU NEED HELP?
Request a Callback Today!
We will usually contact you within 24 hours of your request.