Don't Stuck in the Waiting Room!
Register Online Before You Arrive.
We have up-to-date schedules, contact information, and allow you to make appointments online.
General Introduction
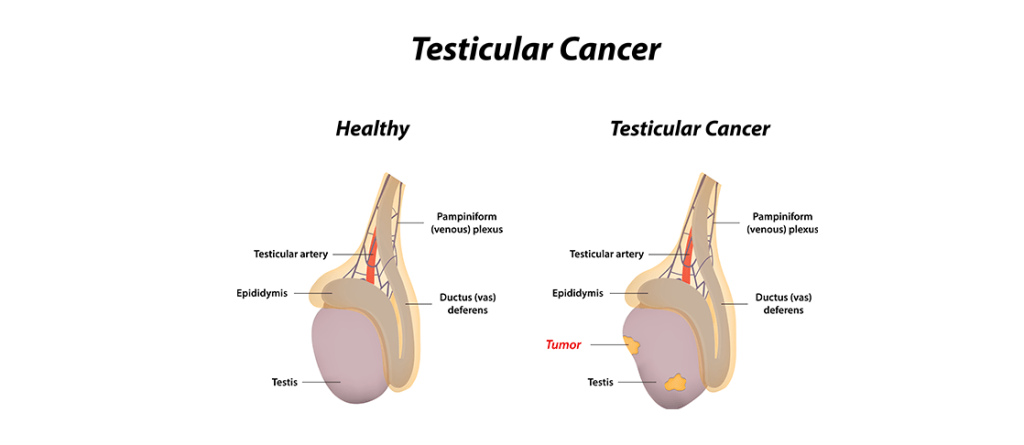
The primary functions of the testes are the production of semen for reproduction and the secretion of the male hormone (testosterone). Although testicular cancer is relatively rare, occurring in only about 1% of men, it is one of the most common types of cancer affecting the organs in men under the age of 35.
For a man with testicular cancer, family history is important. If there is a history of cancer in the father or brother, more attention should be paid, and necessary tests should be done annually without neglect. Most testicular cancers can be treated with surgery and chemotherapy, and recovery rates are generally high. Most testicular cancers arise from cells used in sperm production, called “germ cells.”
Symptoms
The most common sign of testicular cancer is a painless lump in the testicle. Most testicular cancers do not cause pain, but 30 to 40% of patients may experience pain. It is advisable to see a specialist as soon as possible in case of any testicular hardness. Other symptoms of testicular cancer include:
- Enlargement and pain in the breasts
- Back pain
- Neck pain or lump
- Unintentional weight loss and fatigue
Although the exact cause of testicular cancer is unknown, certain factors are associated with it. Risk factors include:
- Cryptorchidism (Undescended Testicle): Patients with this congenital structural disorder have a 4 to 8 times higher chance of developing testicular cancer.
- History of Testicular Cancer: Individuals who have previously had testicular cancer are at a higher risk of developing a second testicular cancer compared to those without such a history.
- Genetic Factors: Individuals with family members with Klinefelter Syndrome, as well as certain genetic disorders such as Down syndrome or androgen insensitivity syndrome, have an increased risk of testicular cancer.
- Age: Most cancers occur after puberty and in men younger than 40, but a second group of men aged 50 to 60 are also at risk for testicular cancer.
- Marijuana Use: Marijuana use has been shown to increase the incidence of testicular cancer.
- Family History: Individuals with first-degree relatives who have had testicular cancer have an increased risk of developing the disease.
Early Diagnosis
Although no screening method has been developed for testicular cancer, individuals are advised to perform self-examinations at regular intervals and consult a doctor if they detect a lump in their testicles.
Diagnostic Methods
Some methods used to support the diagnosis of testicular masses suspected to be cancerous include:
- Scrotal Ultrasound: An imaging method used to determine whether the palpable mass in the testicle originates from the testicle itself or surrounding tissues.
- Blood Tests: Elevated levels of testicular cancer tumor markers such as alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (hCG), and lactate dehydrogenase (LDH) strongly indicate testicular cancer. However, it should be noted that the absence of these markers does not rule out cancer.
- Computed Tomography (CT): An imaging method used to check whether the cancer has spread to surrounding and distant tissues when testicular cancer is detected.
If suspicion of testicular cancer arises following examinations and tests, the removal of the testicle is necessary to confirm the diagnosis.
Treatment Methods
Both the diagnosis and treatment of testicular cancer require the removal of the testicle through a surgical procedure called inguinal orchiectomy, performed through the groin.
- Surgical Treatment: In men with advanced or high-risk cancer, retroperitoneal lymph node dissection (a surgical procedure to remove abdominal lymph nodes) may be recommended.
- Chemotherapy: Chemotherapy drugs can be applied to treat cancer cells that have spread outside the testicles. Additionally, chemotherapy may be applied as an adjunctive treatment in some patients following surgery.
- Radiation Therapy: In some patients with testicular cancer, radiation therapy may be considered a treatment method alongside chemotherapy or surgical operations. It can also be used in patients with metastases or those unsuitable for surgery in combination with chemotherapy.
DO YOU NEED HELP?
Request a Callback Today!
We will usually contact you within 24 hours of your request.